On behalf of our more than 500 member organizations in the field of health and human services, Advocates for Ohio’s Future would like to thank the Ohio General Assembly for recognizing the importance of providing for the safety, health, and well-being of all those they represent.
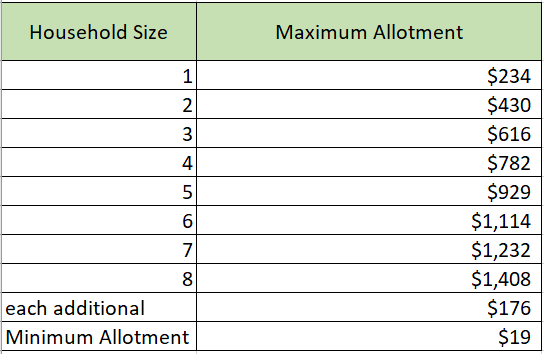
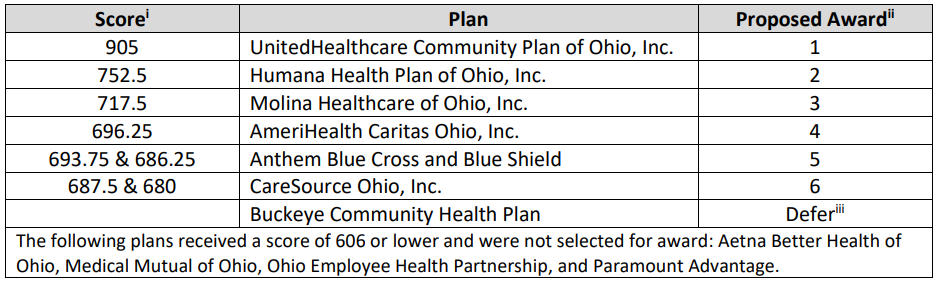
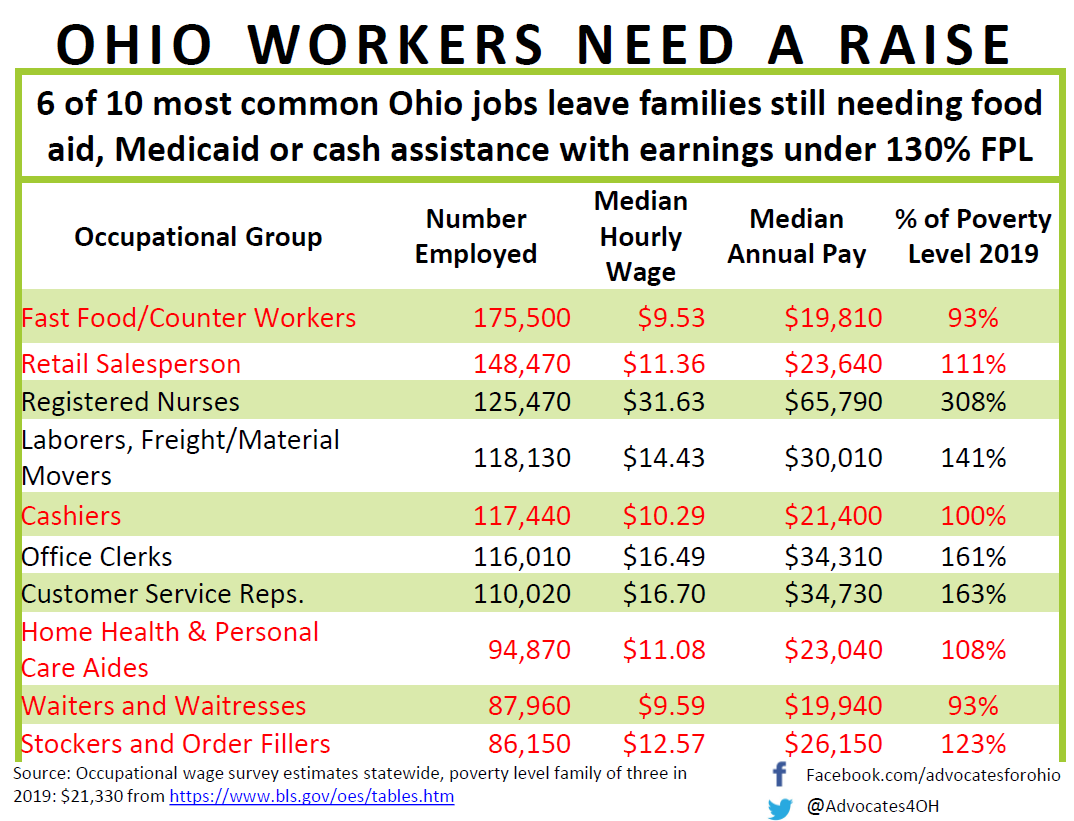
Actions taken through the Conference Committee process and affirmed by Governor DeWine removed provisions that would have terminated the Medicaid managed care procurement process and derailed crucial efforts to refocus, improve, and personalize Medicaid services for Ohioans. The removal of asset testing and other changes targeting the Supplemental Nutrition Assistance Program (SNAP) has ensured that low-income Ohioans will not be forced to choose between having food and owning a car to get to work or saving for an emergency. In addition, this final budget reinstates $250 million in funding for broadband expansion and allows municipal governments to participate in the all-hands-on-deck approach necessary to give every Ohioan the ability to effectively do their job, finish their school assignments, or receive health care when they need it the most.
Unfortunately, the provision that would allow medical practitioners or health care institutions to decline to perform any health care service that violates their conscience as informed by their moral, ethical, or religious beliefs or principles remains in the bill and is signed into law. We are critically concerned about the impact the clause will have on medically underserved Ohioans. LGBTQ+ Ohioans and other members of communities who already don’t seek health care due to perceived or actual bias against them could be denied care under this added language and many will stay home rather than seek needed care. This provision will widen disparities we already have in our health care system.
While there is always room for improvement, the legislature made the decision to remove budget provisions that could have been devastating for many of Ohio’s most vulnerable populations. As a coalition of health and human services organizations, many of our members see daily how these programs have held families together and supported their most basic needs.
We’d like to thank Governor DeWine, Senate President Huffman, Speaker Cupp, Chairman Dolan, Chairman Oelslager and the other members of Conference Committee and the General Assembly for their hard work to finalize the state budget and for investing in our state’s most valuable resource—our people.
We asked you to do better, and you have done so for your constituents. We look forward to continuing our work with you to improve the health and livelihoods of Ohioans into the future.