Last week, the Ohio Department of Medicaid announced the six health care companies that were selected as part of an overhaul of Ohio’s $20 billion managed care system, in the culmination of a procurement process that has lasted more than two years and has been touted as the largest contract in Ohio state history.
UnitedHealthcare Community Plan, Humana, Molina Healthcare, AmeriHealth Caritas, Anthem Blue Cross and Blue Shield, and CareSource will be part of Ohio’s sweeping Medicaid managed care reform, which will work to re-focus the managed care system on the 3 million Ohioans with Medicaid coverage, rather than on the business of managed care.
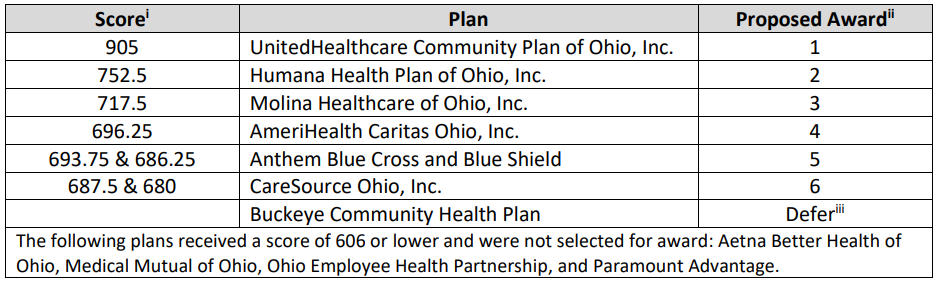
ODM scoring of the six awarded contracts
Medicaid enrollees will continue to have coverage through their current plan until the 2021 open enrollment period this summer, when members can select a new plan to begin coverage in early 2022.
Buckeye Community Health Plan’s bid decision has been deferred, and Aetna Better Health of Ohio and Paramount Advantage, both of which are current Ohio Medicaid managed care organizations, were not awarded contracts.
Ohio Medicaid’s next generation program will also include program coordination with OhioRISE (Resilience through Integrated Systems and Excellence), a managed care program designed to serve Ohio youth with complex behavioral health and multi-system needs. Earlier this month, ODM announced that Aetna Better Health of Ohio would serve as the managed care organization for the OhioRISE program.
Ohio’s current health care system leaves gaps in care for youth with complex needs. It’s estimated that each day, 140 Ohio kids live out of state to access needed behavioral health care, at a cost to the state of $1,100 per day. Some families of youth with complex needs voluntarily relinquish custody of their child as a last resort for their child to receive the expensive, multi-system care needed.
Through OhioRISE, Aetna Better Health will create coordinated services across multiple state agencies, and will expand access to in-home and community-based services to prevent the need for voluntary custody relinquishment and better support Ohio’s children. Ohio will aim to enroll between 55,000 and 60,000 Medicaid-eligible children, up to age 21, in OhioRISE.
by: Sarah Hudacek, AOF Policy Assistant